Sally Brown, University of Washington
That all changed in Seattle a few weeks back. And the rest of the country has quickly followed suit.
Last July, I did a library called Summer Pandemic, making fun of those summer blockbuster movies. It featured articles by Ian Pepper about the fate of various exotic diseases in wastewater and biosolids. Article #3 was about coronaviruses.
We are now living in the movie.
This library provides additional articles on the fate of coronaviruses in wastewater treatment. Remember here that COVID-19 is a new type of coronavirus. What has been reported before for this type of virus is likely to apply to COVID-19, but there are also likely some differences. This is all new and happening fast. Hopefully, some background will help.
First, the basics. With wastewater treatment and biosolids, we have typically focused on disease causing bacteria. With bacteria it is a question of good guys versus bad guys. There are a lot of great bacteria; our bodies are full of them. There are a few bad bacteria. When we are attacked by the bad, it is our good army versus their bad army.
We use fecal coliform or salmonella to measure pathogen kill in biosolids. Below a certain number, their armies are way too weak to cause a problem for the good guys.
Viruses are different. It only takes one or two viable bad guys to cause problems. They are not living per se, but contain DNA or RNA and start making our bodies work against us on entry. While not quite as well known as Lord of the Rings, I would strongly recommend watching Osmosis Jones, both for a good laugh and to better understand the way a virus can work.
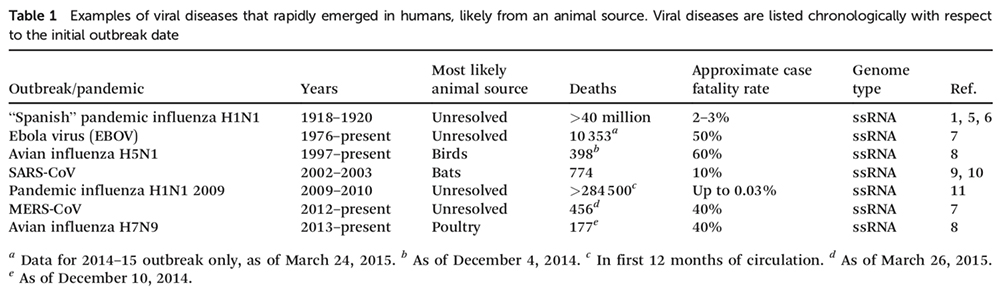
The library starts with a great overview article (Emerging investigators series: the source and fate of pandemic viruses in the urban water cycle). Corona viruses are a subset of viruses that contain the meat of the virus, the DNA or RNA inside an outer protective shell or an envelope. A lot of recent outbreaks fall into this category, including SARS, MERS and Ebola. SARS and MERs are both coronaviruses. A table from the article shows the different viruses that have come from animal sources and their fatality rates.
In general, these viruses are not considered a threat for wastewater or wastewater treatment as most degrade easily and quickly in water. However, there are exceptions. Some avian flu viruses and some coronaviruses are able to persist in water. The authors make a critical point — for these viruses to be a concern for wastewater treatment systems, they have to enter those systems. To do so people would need to shed the viruses in urine, feces or vomit. These viruses that give you the runs are enteric viruses, ones that multiply in the gut and are transmitted through products of our guts. COVID-19 and all coronaviruses have a different outer structure than enteric viruses and are more susceptible to deactivation in water. These are also primarily respiratory viruses; they prefer your lungs to your gut. The main way that they can get into wastewater is if you swallow your snot. Put in more scientific terminology ‘the presence of respiratory virus genes in feces is thought to stem from a patient swallowing virus-laden nasal secretions.’
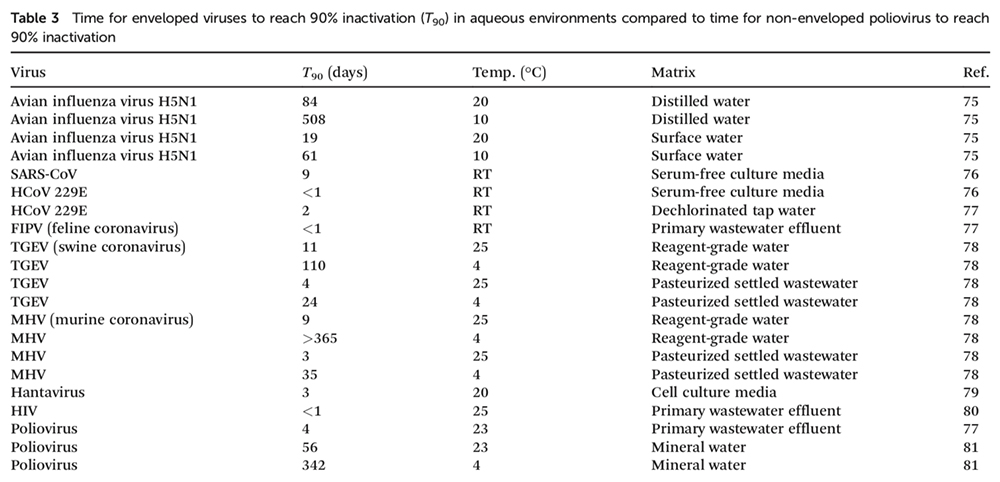
The authors also point out here that just because you can find the DNA or RNA of a virus in wastewater, it doesn’t mean that the virus is active. An intact and entire particle is required to be of concern. There is a section on coronaviruses with a focus on SARS. SARS was unique because although primarily a respiratory virus, diarrhea occurred in a portion of infected individuals. The other prior coronaviruses have not had a significant presence in fecal material. From what I’ve read about COVID-19, it is primarily a respiratory virus with little in the way of gastrointestinal symptoms being reported. Here is another table from the paper with survivability of different viruses in aqueous environments.
The article goes on to talk about persistence of different viruses in wastewater and issues with quantifying viruses. We’ll get to those topics later.
Next article is an in depth look at the SARS virus (Enteric involvement of severe acute respiratory syndrome–associated coronavirus infection). SARS is of interest here, as it is a coronavirus just like COVID 19. However, it is different from COVID-19 in two critical ways: the % mortality is much higher, and it is often accompanied by diarrhea. In fact, SARS was spread in one cluster (an apartment building in Hong Kong) through poorly constructed plumbing. Aerosolized fecal matter is what got them. This article talks about the presence of the virus in the intestinal tracts of victims, the prevalence of diarrhea (20%), and replication in the intestinal tract. In fact,the Ian Pepper paper on coronaviruses (July library) was a study on persistence in wastewater of other viruses used as surrogates for SARS.
From here we go to the sky is falling paper (Identification of viral pathogen diversity in sewage sludge by metagenome analysis). Here the authors use metagenomics to test for DNA/ RNA presence of a wide range of viruses in wastewater and sludge. They found plenty of them, including coronaviruses. The authors collected wastewater from different regions in the US and different sized plants and scoured the samples for virus DNA. The authors identified over 400,000 contiguous sequences of genetic data. Of those, 0.11% were likely associated with human viral pathogens. The most common viruses were- no surprises here- herpes and HPV. A reason to get the vaccine and wear a condom. Coronaviruses were also relatively common, found in 83% of the tested samples. The results are shown below.
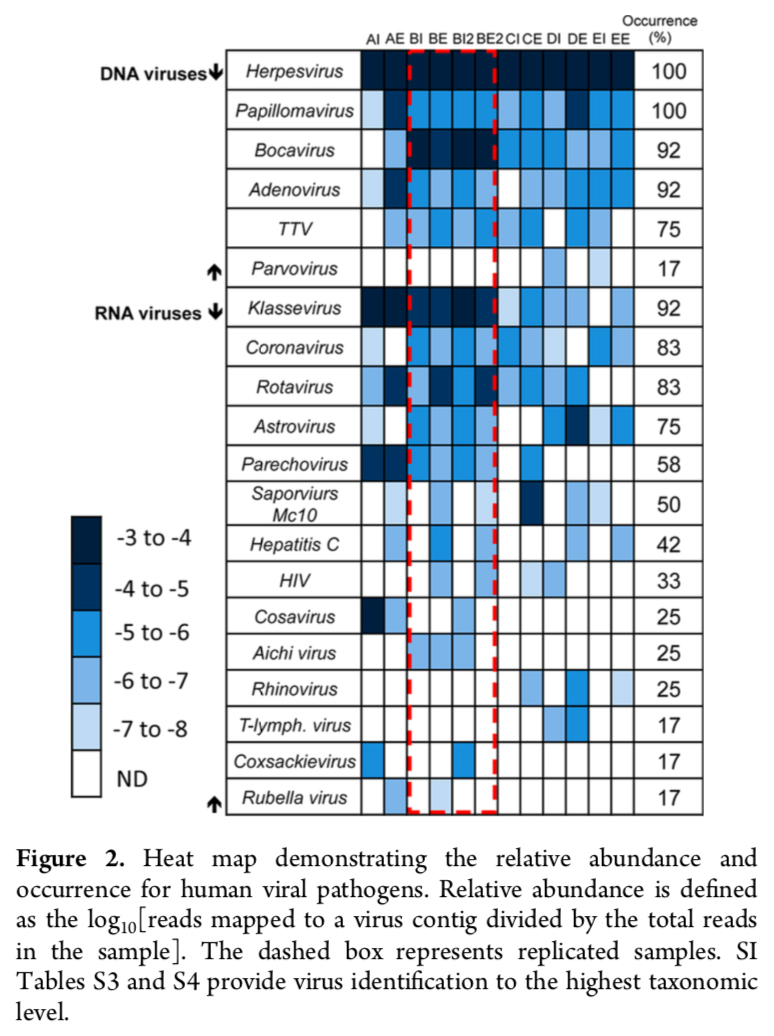
What is critical to remember here, and was discussed in the first paper, is that sequencing to find viruses does not have any relation to the viability of those viruses. So, cry wolf all you want, let’s look at viability of coronaviruses in the last two papers in the library.
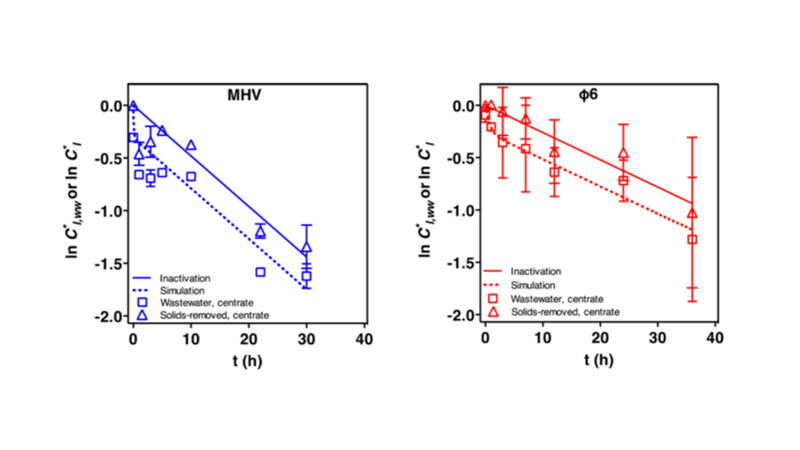
The 4th paper is by the same group that wrote the first paper (Survivability, partitioning, and recovery of enveloped viruses inuntreated municipal wastewater). It specifically addresses survivability of enveloped (includes corona) viruses in untreated municipal wastewater. They used two model enveloped viruses and two bacteriophages (viruses that infect bacteria). In unpasteurized wastewater at 25 C the two enveloped viruses lasted for 7 and 13 hours. Cool that water down and the viruses last a lot longer; 28-36 hours. Pasteurizing the water also slowed down the deactivation. The authors also found that the majority of the viruses partitioned to the liquids rather than the solids. When spiked into water containing solids, a rapid decrease was seen in the first hour. This means that viruses entering the plant in cooler climates may be active but they are almost certainly inactive in the solids and very likely inactive in the effluent. Below is the graph showing the decline of the two enveloped surrogates that they used.
The final paper (Inactivation of an enveloped surrogate virus in human sewage) confirms the results from the 4th paper. The hotter the better, but lifespan is days rather than weeks.
The take-home from these studies and from the previous library is that, because of a number of factors, wastewater and biosolids are not going to be a realistic concern for transmission of COVID-19. I hope that this is of some help/hope and that soon we can all get back to worrying about PFAS.
Remember to social distance and to wash your hands!